When your kidneys, the body's meticulous filters, start to fail, the effects ripple through your entire system. A key condition indicating this failure is nephrotic syndrome, a collection of debilitating symptoms caused by massive protein loss in the urine. One of the most aggressive and challenging diseases that leads to this outcome is Focal Segmental Glomerulosclerosis (FSGS).
At Neph Cure Inc., we believe that understanding the root cause of kidney disease is the first, most crucial step toward effective treatment. Modern science is illuminating the complex genetic and immunological pathways that lead to FSGS, particularly focusing on the role of the APOL1 gene kidney disease causes of focal segmental glomerulosclerosis.
This professional post will explore the key nephrotic syndrome symptoms, detail the multi-faceted nature of FSGS, and highlight the powerful and specific influence of the APOL1 gene in driving this devastating disease. We are committed to translating this complex science into clear, actionable knowledge for you.
Part 1: The Widespread Impact—Nephrotic Syndrome Symptoms
Nephrotic syndrome is a clinical diagnosis, meaning it’s a group of symptoms and signs that collectively point to severely damaged glomerular filters. When the kidney's podocytes are compromised, the filtration barrier becomes "leaky," allowing large, essential proteins—primarily albumin—to escape into the urine.
The Four Hallmarks of Nephrotic Syndrome
Monitoring these nephrotic syndrome symptoms is essential for assessing disease activity and the effectiveness of treatment:
Massive Proteinuria (Foamy Urine): This is the defining feature. The loss of vast amounts of protein (over $3.5$ grams per $1.73\text{m}^2$ daily) makes the urine persistently frothy or foamy, much like beer foam.
Edema (Severe Swelling): This is the most visible and often the first symptom noticed. It occurs because the loss of albumin in the blood (hypoalbuminemia) lowers the blood's osmotic pressure, causing fluid to leak out of the blood vessels and accumulate in the tissues. Swelling is typically prominent in the ankles, feet, and face (especially around the eyes).
Hypoalbuminemia: Low levels of albumin in the blood (typically below $3.0 \text{g/dL}$), which directly drives the edema.
Hyperlipidemia: Elevated levels of cholesterol and triglycerides. The liver attempts to compensate for the lost proteins by increasing protein production, which includes lipoproteins (fats).
In addition to these core symptoms, patients often experience fatigue, increased risk of infection (due to the loss of immune proteins), and increased risk of blood clots (due to the loss of anti-clotting proteins).
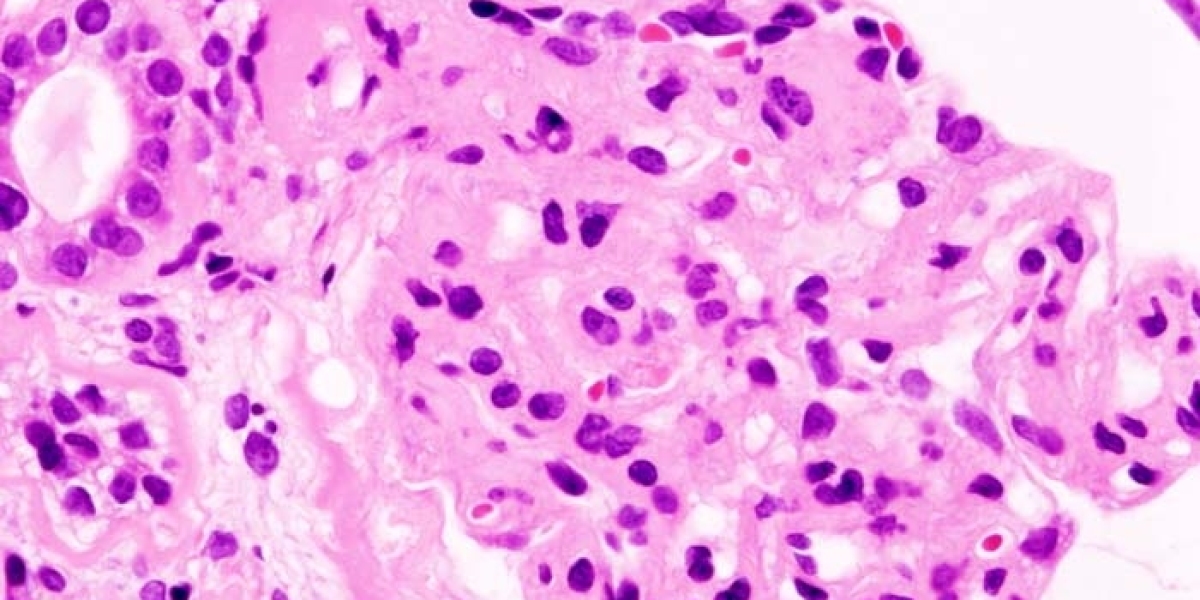
Part 2: The Pathology of Scarring—Focal Segmental Glomerulosclerosis
Focal Segmental Glomerulosclerosis (FSGS) is one of the most common pathologies leading to nephrotic syndrome and is characterized by scarring (sclerosis) in segments of some (focal) but not all glomeruli. It is a leading cause of end-stage renal disease (ESRD).
FSGS is not a single disease but a pattern of injury that has three primary, distinct origins:
The Types of FSGS
Primary (Idiopathic) FSGS: The cause is unknown, but it's strongly suspected that a circulating permeability factor—an unidentified molecule in the blood—attacks the podocytes, causing them to detach and the glomerulus to scar. This form is often severe and can recur rapidly after a kidney transplant.
Secondary FSGS: Scarring occurs as an adaptive response to known stressors. This includes:
Hyperfiltration Injury: When a patient loses kidney tissue (e.g., from prior injury or a single kidney), the remaining healthy glomeruli are forced to work harder, leading to stress, injury, and eventual scarring.
Systemic Diseases: FSGS secondary to severe obesity, uncontrolled hypertension, or diabetes.
Genetic FSGS: Caused by inherited mutations in genes that code for podocyte structural proteins. This is where the APOL1 gene plays a critical, distinct role.
Part 3: The Genetic Accelerator—APOL1 Gene Kidney Disease Causes of Focal Segmental Glomerulosclerosis
The identification of the high-risk variants of the APOL1 gene has revolutionized the causes of focal segmental glomerulosclerosis, particularly for individuals of recent African descent. This gene, which evolved to protect against African sleeping sickness, has specific variants (G1 and G2) that are now recognized as a major genetic risk factor for aggressive kidney disease.
APOL1 and FSGS: The Double-Hit Hypothesis
Having two high-risk APOL1 alleles (one inherited from each parent) does not automatically guarantee disease, but it significantly elevates the risk and severity when a "second hit" (e.g., an infection, a concurrent illness, or chronic stress) occurs. The APOL1 gene kidney disease causes of focal segmental glomerulosclerosis are linked to its toxic effect on the podocyte:
Toxicity Mechanism: The high-risk APOL1 protein variants are believed to form toxic pores or channels in the membrane of the podocytes. This causes cellular stress, damage, and ultimately death, leading directly to the scarring pattern seen in FSGS.
Aggressive Disease: FSGS linked to APOL1 risk variants is known to be particularly aggressive, progressing faster toward end-stage renal disease (ESRD) compared to other forms of the disease.
Disease Association: Beyond typical idiopathic FSGS, the high-risk APOL1 variants are strongly associated with other severe forms of kidney damage, including HIV-Associated Nephropathy (HIVAN) and accelerated hypertensive nephrosclerosis.
Part 4: The Need for Precision in FSGS Management
Understanding the APOL1 gene kidney disease causes of focal segmental glomerulosclerosis is no longer academic; it is critical for guiding clinical decisions.
Treatment Selection: Patients with genetic FSGS (including those due to APOL1) often do not respond to the immunosuppressive therapies (like steroids or calcineurin inhibitors) used for Primary FSGS. Kidney disease genetic testing for APOL1 allows physicians to avoid unnecessary, toxic treatments.
Transplant Risk: Knowing the APOL1 status helps predict recurrence risk after a kidney transplant. If the disease is purely genetic, the recurrence risk is extremely low. However, if the transplant recipient carries the high-risk genes and receives a kidney from a donor who also carries the high-risk genes, the donor kidney may be more vulnerable to damage.
Future Therapies: The understanding that APOL1 toxicity is a key driver has spurred the development of targeted APOL1 inhibitor drugs—small molecules designed to block the toxic function of the protein. This is the future of precision FSGS kidney disease treatment.
Neph Cure Inc.: Advocating for Targeted Solutions
Living with nephrotic syndrome symptoms caused by a challenging disease like FSGS demands clarity and hope. At Neph Cure Inc., we are dedicated to ensuring that every patient benefits from the breakthroughs in genetic and molecular science.
The discovery of the APOL1 gene kidney disease causes of focal segmental glomerulosclerosis is a landmark moment, providing a molecular explanation for a disease that disproportionately affects millions and accelerating the development of the first truly targeted therapies.
We are committed to empowering patients through comprehensive testing, education on the latest research (including APOL1 inhibitors), and advocacy for personalized medicine approaches that will finally treat the cause, not just the symptoms.
Ready to explore how advanced genetics can inform your kidney care strategy?
Contact Neph Cure Inc. today to learn about the latest in FSGS diagnostics and emerging APOL1 targeted therapies.